

 2021-09-02
2021-09-02
Abstract
We investigated the effects of pravastatin, a competitive inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, on interstitial inflammation and fibrosis, using an animal model of chronic cyclosporine A (CsA)-induced nephropathy. Sprague-Dawley rats were maintained on a low-salt diet (0.05% sodium) and treated daily for 1 or 4 wk with vehicle (olive oil; 1 ml/kg sc), CsA (15 mg/kg sc), or both CsA and pravastatin (5 or 20 mg/kg in the drinking water). Anti-inflammatory and antifibrotic effects of pravastatin were studied by evaluating the concentrations of the inflammatory mediators osteopontin (OPN) and C-reactive protein (CRP), of fibrotic cytokine-transforming growth factor (TGF)-β1, and the presence of ED-1-positive cells (macrophages). In addition, renal function, serum lipid levels, histopathology (arteriolopathy and tubulointerstitial fibrosis), and the expression of the vasoactive factors endothelial nitric oxide synthase (eNOS) and renin protein were also compared for different treatment groups. Pravastatin induced dose-dependent decreases in the expression of OPN, intrarenal CRP, and TGF-β1, and in the numbers of ED-1-positive cells at 1 and 4 wk. These were accompanied by a significant attenuation of tubulointerstitial fibrosis at 4 wk. The downregulation of eNOS protein expression in CsA-treated rat kidney was markedly upregulated by pravastatin treatment, although intrarenal renin expression was unaffected. Renal dysfunction induced by CsA significantly improved with administration of pravastatin at a dose of 20 mg/kg. Neither CsA nor pravastatin influenced serum lipid or high-sensitivity CRP levels in the treatment groups. Thus in chronic CsA nephropathy, pravastatin effectively abrogates the progression of tubulointerstitial inflammation and fibrosis. This may support the clinical use of pravastatin.
chronic cyclosporine a (CsA)-induced nephropathy is characterized by progressive renal insufficiency, afferent arteriolopathy, tubulointerstitial inflammation, and striped fibrosis (36). The mechanisms leading to chronic CsA-induced nephropathy are not fully understood. However, utilizing a well-established animal model, we have previously demonstrated, as have others, that a complex causative network may involve inflammatory mediators (30, 42), transforming growth factor (TGF)-β1 (49, 54), the renin-angiotensin system (RAS) (3, 55), and nitric oxide (NO)/NO synthase (NOS) (1, 56).
Interstitial inflammation is the predominant feature of chronic CsA nephropathy that precedes fibrosis (59). Osteopontin (OPN) is a potent chemoattractant and adhesion molecule for monocytes and macrophages, and there is overwhelming evidence that the upregulation of tubular OPN expression is closely associated with macrophage influx and renal scarring in a wide range of kidney diseases including chronic CsA-induced nephropathy (12, 22, 30, 31, 60). This concept is supported by studies using OPN knockout mice or anti-OPN antibody-treated animals (34, 40). TGF-β1, a well-known profibrogenic cytokine, has been implicated in the fibrosis of chronic CsA nephropathy, probably via its effects on extracellular matrix synthesis and degradation (48). Administration of neutralizing anti-TGF-β antibody thus improves CsA-induced renal dysfunction and structural damage (32).
Statins are competitive inhibitors of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, the key enzyme that regulates the synthesis of cholesterol from mevalonic acid by suppressing the conversion of HMG-CoA (13). Because of this activity, the clinical use of statins has produced a significant reduction in cardiovascular-related morbidity and mortality in patients with established cardiovascular disease and hypercholesterolemia (4, 47). However, mevalonate is the precursor not only of cholesterol but also of many nonsteroidal compounds; inhibition of HMG-CoA reductase by statins may therefore result in pleiotropic effects (8, 46). Statins may thus exert anti-inflammatory and antiarteriosclerotic actions beyond lipid reduction (37). The renoprotective effects of statins have also been reported in ischemia-reperfusion injury (21), subtotal renal ablation (29), streptozotocin-induced diabetic nephropathy (25), puromycin-induced nephrosis (15), and unilateral ureteral obstruction (35). Nevertheless, the benefits of statins in a rat model of chronic CsA-induced nephropathy have yet to be reported.
We hypothesized that statins may have anti-inflammatory and antifibrotic effects on chronic CsA-induced nephropathy. To test this hypothesis, we investigated the effects of pravastatin on inflammatory mediators and profibrotic cytokine in a well-described rat model of chronic CsA-induced nephropathy.
MATERIALS AND METHODS
Animals and drugs. Male Sprague-Dawley rats (Charles River Technology), initially weighing 200 to 220 g, were housed in cages in a temperature- and light-controlled environment and allowed free access to a low-salt diet (0.05% sodium, Teklad Premier, Madison, WI) and tap water. Cyclosporine (Novartis Pharma, Basle, Switzerland) was diluted in olive oil to a final concentration of 15 mg/ml. Pravastatin sodium (Bristol-Myers Squibb Pharmaceutical) was dissolved in drinking water and administered at two doses of 5 or 20 mg/kg. This dosage and method of pravastatin administration were chosen according to previous reports showing that pravastatin at a dose of 20 mg/kg did not alter blood lipid levels (7, 9).
Experimental design. The experimental protocol was approved by the Animal Care Committee of the Catholic University of Korea. Rats were randomized into six groups and treated daily for 1 or 4 wk as follows:
1. Vehicle (VH; n = 6): subcutaneous injection with olive oil (1 ml/kg).
2. Vehicle plus pravastatin (VH+P5; n = 6): simultaneous treatment with olive oil and pravastatin (5 mg/kg in drinking water).
3. Vehicle plus pravastatin (VH+P20; n = 6): simultaneous treatment with olive oil and pravastatin (20 mg/kg in drinking water).
4. CsA (n = 6): subcutaneous injection with CsA (15 mg/kg).
5. CsA plus pravastatin (CsA+P5; n = 8): simultaneous treatment with CsA and pravastatin (5 mg/kg).
6. CsA plus pravastatin (CsA+P20; n = 8): simultaneous treatment with CsA and pravastatin (20 mg/kg).
Animals were euthanized under ketamine anesthesia at 1 or 4 wk, and the kidneys were rapidly removed for morphological and molecular studies.
Renal function. Before death, animals were individually housed in metabolic cages (Tecniplast Gazzada, Beguggiate, Italy) for 24-h urine collection, and blood samples were obtained to evaluate serum creatinine (Scr). The creatinine clearance rate (Ccr) was calculated with the standard formula.
Miscellaneous measurements. After the treatment was started, rats were pair-fed and daily body weight was monitored. Systolic blood pressure was recorded in conscious rats by the tail-cuff method with plethysmography using a tail manometer-tachometer system (BP-2000, Visitech system, Apex); at least three readings for each rat were averaged. Whole blood CsA levels were measured by a monoclonal radioimmunoassay (Incstar, Stillwater, MN). Serum total cholesterol and triglycerides levels were determined with an auto-analyzer (Coulter-STKS, Coulter Electronics). High-sensitivity C-reactive protein (hs-CRP) was measured by a particle-enhanced immunoturbidometric method using a Cobas Integra 700 (Roche Diagnostic System, Basel, Switzerland) (5).
Histopathology. Kidney tissues were fixed in periodate-lysineparaformaldehyde (PLP) solution and embedded in wax. After dewaxing, 4-μm sections were processed and stained with periodic acid-Schiff or Masson's trichrome and hematoxylin. Arteriolopathy of the afferent arterioles was manifested by expansion of the cell cytoplasm of terminal arteriolar smooth muscle cells by eosinophilic, granular material and semiquantitatively evaluated by counting the percentage of juxtaglomerular afferent arterioles with arteriolopathy per total number of juxtaglomerular afferent arterioles available for examination, using a ×20 objective; at least 60 glomeruli were assessed per specimen. A finding of tubulointerstitial fibrosis (TIF) was defined as a matrix-rich expansion of the interstitium with tubular dilatation, tubular atrophy, tubular cast formation, sloughing of tubular epithelial cells, or thickening of the tubular basement membrane. A minimum of 20 fields/section was assessed using a color image analyzer (TDI Scope Eye Version 3.0 for Windows, Olympus). Briefly, the image was captured, and the extent of TIF was quantified using the Polygon program by counting the percentage of areas injured per field of cortex under ×100 magnification. Histopathological analyses were performed in randomly selected cortical fields of sections by a pathologist blinded to the identity of the treatment groups.
Immunohistochemistry. After dewaxing, sections were incubated with 0.5% Triton X-100/PBS solution for 30 min and washed three times with PBS. Nonspecific binding sites were blocked with normal horse serum diluted 1:10 in 0.3% BSA for 30–60 min and then incubated for 2 h at 4°C in mouse antiserum against OPN (MPIIIB10; obtained from the Developmental Studies Hybridoma Bank, Univ. of Iowa, Iowa City, IA) diluted in 1:1,000 in a humid environment. After being rinsed in Tris-buffered saline (TBS), sections were incubated in peroxidase-conjugated rabbit anti-mouse IgG (Amersham Pharmacia Biotech, Piscataway, NJ) for 30 min. For coloration, sections were incubated with a mixture of 0.05% 3,3′-diaminobenzidine containing 0.01% H2O2 at room temperature until a brown color was visible, washed with TBS, counterstained with hematoxylin, and examined under light microscopy. The procedure of immunostaining for ED-1 (Serotec), CRP (Sigma), and renin was similar to that for OPN. The antibody against renin was kindly provided by Dr. Kirsten Madsen (Dept. of Medicine, Univ. of Florida, Gainesville, FL). This antibody is known to recognize rat renin and prorenin (39). In addition, immunohistochemistry for TGF-β1 (Santa Cruz Biotechnology, Santa Cruz, CA) was performed in cryostat sections. The number of ED-1- or CRP-positive cells was counted in at least 20 fields of cortex/section under ×200 magnification, and renin-positive glomeruli were evaluated by counting a minimum of 50 glomeruli/specimen.
Immunoblotting. For immunoblotting analysis, kidney cortex tissue was homogenized in lysis buffer [20 mM/l Tris·Cl (pH 7.6), 150 mM/l NaCl, 1% wt/vol sodium deoxycholate, 1% vol/vol Triton X-100, 0.1% SDS, 2 mM/l NaVO3, and freshly added 1% vol/vol aprotinin, leupeptin (1 μg/ml), pepstatin (1 μg/ml), and 1 mM PMSF]. Homogenates were centrifuged at 3,000 rpm for 15 min at 4°C, and the protein concentration of the lysate was determined using a protein microassay of the Bradford method (Bio-RAD, Hercules, CA). Protein samples were resolved on 15% SDS-PAGE gels and then electroblotted onto Bio-Blot nitrocellulose membrane (Bio-Rad). An equal amount of protein loading (50 μg) was verified by Ponceau S staining. The membrane was blocked for 1 h in TBS-added Tween 20 [TBS-T; 10 mM Tris·Cl, 150 mM NaCl (pH 8.0), 0.05% Tween 20] containing 5% nonfat powdered milk. Endothelial NOS (eNOS) was detected by incubation for 1 h with a monoclonal anti-eNOS antibody (Transduction Laboratories) diluted 1:1,000. Primary antibody incubation was followed by six washes with TBS-T. The blot was then incubated with secondary antibody (goat anti-mouse IgG-horseradish peroxidase) conjugate at 1:1,000 (Bio-Rad) for 30 min. Antibody-reactive protein was detected using enhanced chemiluminescence (Amersham Life Science). Optical densities were obtained using the VH group as 100% reference and normalized with β-actin.
Northern blot analysis. A 1-kb cRNA probe was generated from the 2B7 cDNA clone of rat smooth muscle OPN (11). Sense and antisense cRNA probe were labeled with digoxigenin (DIG)-UTP using a T7 RNA polymerase kit (Boehringer Mannheim, Mannheim, Germany). Probes were precipitated, and incorporation of DIG was determined by dot blotting. Northern blotting was performed as previously described by others (60). Briefly, kidney cortex was homogenized. Total RNA was extracted using the RNAzol reagent (TEL-TEST), and 20-μg samples were denatured with glyoxal and dimethylsulphoxide, size fractionated on 1.2% agarose gels, and capillary blotted onto positively charged nylon membranes (Boehringer Mannheim). Membranes were hybridized overnight at 68 or 42°C with DIG-labeled cRNA (or 32P-labeled cDNA probes for TGF-β1) in a DIG wash and Block Buffer Set solution (Boehringer Mannheim). After hybridization, membranes were finally washed in 0.1× SSC/0.1% SDS at 68°C or 0.2× SSC/0.1% SDS at 42°C. Bound probes were detected using sheet anti-DIG antibody (Fab) conjugated with alkaline phosphatase (Boehringer Mannheim) and developed with CSPD-star enhanced chemiluminescence (Boehringer Mannheim). The densitometry analysis was performed using the NIH Image program. Three determinations for each band were averaged and referenced to 18S.
Statistical analysis. Data are expressed as means ± SE. Multiple comparisons among groups were performed by one-way ANOVA with the post hoc Bonferroni test (SPSS software version 9.0, Microsoft). Statistical significance was assumed to be P < 0.05.
RESULTS
Effect of pravastatin on basic parameters in chronic CsA nephropathy.Table 1 summarizes basic parameters for each group. The mean body weight of CsA-treated rats was significantly lower than that for the VH-treated rats (255 ± 5 vs. 295 ± 4 g, P < 0.01). Administration of pravastatin at either dose did not prevent loss of body weight. Systolic blood pressure measured by tail-cuff pressure did not differ significantly among any of the treatment groups throughout the study. Four-week CsA treatment resulted in an increase in blood CsA concentration to a level of 2,617 ± 267 ng/ml, whereas pravastatin did not influence the level of CsA concentration (CsA+P5: 2,742 ± 296 ng/ml; CsA+P20: 2,727 ± 263 ng/ml). There were no significant differences among groups for any of the lipid parameters.
Table 1. Basic parameters in different groups
Effect of pravastatin on renal function in chronic CsA nephropathy. CsA treatment for 1 wk did not cause renal dysfunction (Scr: 0.63 ± 0.12 vs. 0.58 ± 0.11 mg/dl; Ccr: 0.48 ± 0.06 vs. 0.52 ± 0.02 ml·min-1·100 g-1, P > 0.05 vs. VH, respectively). Table 1 shows 4-wk data on renal function in the experimental groups. Daily treatment of rats with CsA for 4 wk caused higher levels of Scr (1.21 ± 0.07 vs. 0.55 ± 0.11 mg/dl, P < 0.01) and lower levels of Ccr (0.15 ± 0.01 vs. 0.53 ± 0.04 ml·min-1·100 g-1, P < 0.01) than in VH-treated rats. Pravastatin at the lower dose of 5 mg/kg did not improve renal function, whereas the higher dose of pravastatin (20 mg/kg) normalized levels of Scr and Ccr compared with CsA or CsA+P5 groups (Scr: 0.78 ± 0.04 mg/dl; Ccr: 0.42 ± 0.04 ml·min-1·100 g-1, P < 0.05, respectively).
Effect of pravastatin on histopathology in chronic CsA nephropathy. CsA-treated rats showed the typical histopathological features of chronic CsA nephrotoxicity (afferent arteriolopathy, striped interstitial fibrosis, and tubular atrophy with focal inflammatory cell accumulation). Afferent arteriolopathy was manifested as the replacement of smooth muscle cells of the afferent glomerular arterioles by periodic acid-Schiff-positive material, resulting in a typical circumferential appearance of the lesion (Fig. 1). In our semiquantitative scoring system, the arteriolopathy was significantly higher in the CsA group than the VH group (28 ± 3 vs. 11 ± 2, P < 0.01), whereas this was markedly decreased with pravastatin treatment compared with the CsA group (CsA+P5: 12 ± 2; CsA+P20: 12 ± 2, P < 0.01 vs. CsA, respectively). CsA treatment for 1 wk did not cause TIF, although macrophage infiltration was observed. On the other hand, a significant increase in the TIF score (Table 2) was found in the CsA group at 4 wk compared with the VH group (35 ± 4 vs. 0 ± 0%, P < 0.01) (Fig. 2). In contrast, the score decreased markedly when pravastatin was administered at the same time (19 ± 2 vs. 35 ± 4%, P < 0.05 vs. CsA), and a further decrease was observed in the CsA+P20 group (11 ± 2 vs. 19 ± 2%, P < 0.05 vs. CsA+P5).
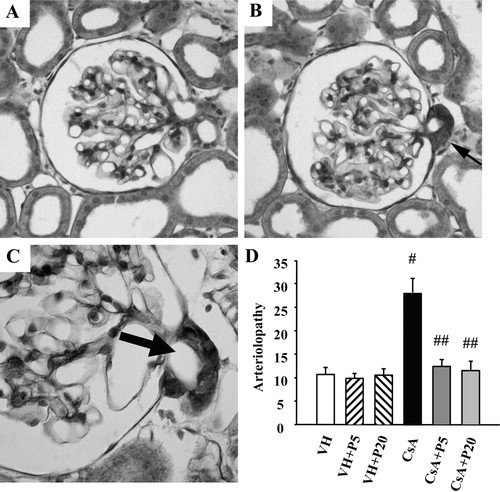
Fig. 1.Representative photomicrographs of arteriolopathy and semiquantitative analysis. A: normal glomerulus. Cyclosporine A (CsA) treatment for 4 wk induces a typical afferent arteriolopathy (B and C). The micrograph shows a glomerulus with expansion of the cell cytoplasm of terminal arteriolar smooth muscle cells by eosinophilic, granular material (arrow). Using semiquantitative analysis, the increased arteriolopathy seen in CsA-treated rat kidneys was significantly reduced with pravastatin administration. Periodic acid-Schiff staining; original magnification: ×400 (A and B); ×1,000 (C). P5 and P20, vehicle (VH) plus 5 and 20 mg/kg in drinking water, respectively.#P < 0.01 vs. VH.##P < 0.01 vs. CsA.
Download figureDownload PowerPoint
Table 2. Histological analyses
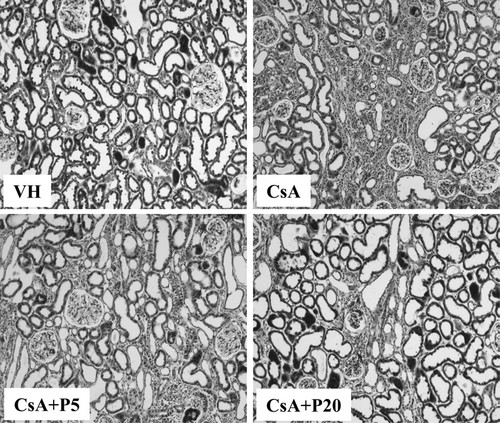
Fig. 2.Representative photomicrographs showing the degree of renal tubulointerstitial fibrosis. CsA treatment for 4 wk induced a typical interstitial fibrosis, inflammatory cell infiltration, and tubular atrophy. Note that pravastatin significantly decreased tubulointerstitial fibrosis in accordance with its dosage. Trichrome stain; original magnification: ×100.
Download figureDownload PowerPoint
Effect of pravastatin on serum hs-CRP and intrarenal CRP expression in chronic CsA-induced nephropathy.Table 1 outlines the hs-CRP concentrations in each group. The mean hs-CRP concentration in the VH group was 0.25 ± 0.04 mg/l. Similarly, the mean hs-CRP in the CsA group was 0.23 ± 0.03 mg/l, and there was no significance in serum hs-CRP between the VH and the CsA groups (P = 0.7 vs. VH). Pravastatin at either dose did not alter the hs-CRP concentrations (CsA+P5: 0.23 ± 0.04 mg/l; CsA+P20: 0.23 ± 0.03 mg/l, P > 0.7 vs. CsA, respectively).
Immunohistochemistry showed a significant increase in CRP expression and immunoreactivity in the CsA-treated rat kidneys, which were confined to cortical tubular epithelial cells (Fig. 3). In our quantitative system (Table 2), the number of CRP-positive cells was dramatically increased in the CsA group compared with the VH group (59 ± 9 vs. 25 ± 3, P < 0.05), whereas their numbers were significantly decreased in the CsA+P group (34 ± 4, P < 0.01 vs. CsA), and a further decrease was observed in the CsA+P20 group (26 ± 2, P < 0.05 vs. CsA+P5). Effect of pravastatin on macrophage infiltration in chronic CsA-induced nephropathy. ED-1-positive cells were detected only rarely in the kidneys of VH-treated animals (Fig. 4, 17 ± 2). CsA treatment increased the number of ED-1-positive cells at 1 and 4 wk (Table 2; 1 wk: 29 ± 7; 4 wk: 89 ± 9, P < 0.01 vs. VH, respectively). Concomitant administration of pravastatin significantly decreased the number of ED-1-positive cells (1 wk: 18 ± 4; 4 wk: 62 ± 6, P < 0.01 vs. CsA, respectively), and this decrease was more pronounced with 20 mg/kg pravastatin administration compared with the CsA+P5 group (1 wk: 10 ± 3; 4 wk: 39 ± 11, P < 0.05, respectively).

Fig. 3.Representative photomicrographs of immunohistochemistry for C-reactive protein (CRP). A: VH-treated rat kidneys. CsA treatment led to a significant increase in CRP immunoreactivity (arrows, B and C). Pravastatin decreased CRP immunoreactivity in accordance with dosage (CsA+P20; D). Immunohistochemical staining; original magnification: ×400 (A, B, and D); ×1,000 (C).
Download figureDownload PowerPoint
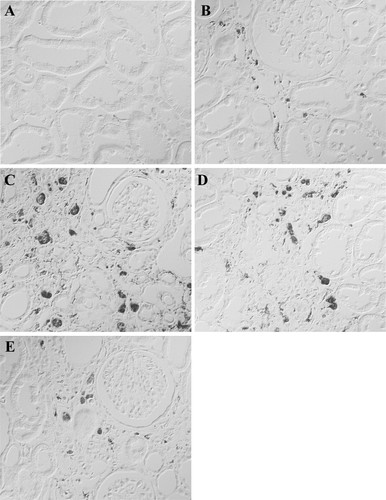
Fig. 4.Representative photomicrographs of immunohistochemistry for ED-1. ED-1-positive cells (macrophages) were rarely observed in VH-treated rat kidney (A), but their numbers increased with CsA treatment for 1 wk (B), and a further increase was observed at 4 wk (C). Pravastatin treatment [CsA+P5 (D); CsA+P20 (E)] significantly decreased ED-1-positive cells in accordance with dosage at 4 wk. Immunohistochemical staining; original magnification: ×400.
Download figureDownload PowerPoint
Effect of pravastatin on OPN mRNA and protein expression in chronic CsA-induced nephropathy. Northern blot analysis of the kidney cortex revealed a dramatic increase in OPN mRNA in the CsA group at 1 (956 ± 117 vs. 109 ± 17, P < 0.01) and 4 wk (1,578 ± 43 vs. 116 ± 6, P < 0.01) compared with the VH group (Fig. 5). Pravastatin dose dependently suppressed OPN mRNA expression at 1 (CsA+P5: 423 ± 168, P < 0.05 vs. CsA; CsA+P20: 197 ± 63, P < 0.05 vs. CsA+P5, respectively) and 4 wk (CsA+P5, 1,037 ± 75, P < 0.05 vs. CsA; CsA+P20, 696 ± 53, P < 0.05 vs. CsA+P5, respectively). Immunohistochemistry consistently revealed that most cortical structures were negative for OPN. In contrast, the expressions of OPN protein were dramatically higher in tubular epithelial and Bowman's capsule cells in CsA-treated rats (Fig. 6). The most striking changes were seen in the renal cortex, which normally expresses very little constitutive OPN. It is notable that the sites of strong OPN protein expression were in areas of inflammatory cell infiltration and severe TIF. In the CsA+P groups, the upregulated OPN protein levels decreased significantly.
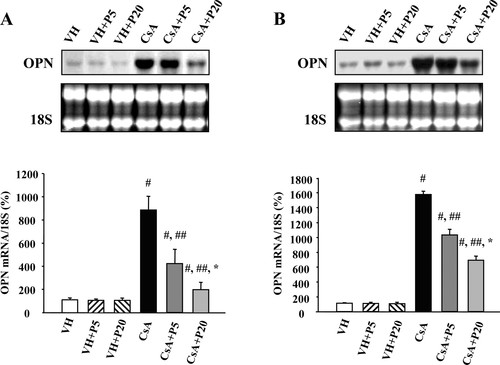
Fig. 5.Northern blotting and quantitative analysis of osteopontin (OPN) mRNA expression. OPN mRNA expression was significantly increased in rat kidneys with CsA treatment at 1 or 4 wk, whereas pravastatin markedly decreased its expression in a dose-dependent manner. Relative OPN mRNAs values are represented with the VH group designated as 100% reference and are normalized to 18S.#P < 0.01 vs. VH.##P < 0.01 vs. CsA. *P < 0.05 vs. CsA+P5.
Download figureDownload PowerPoint
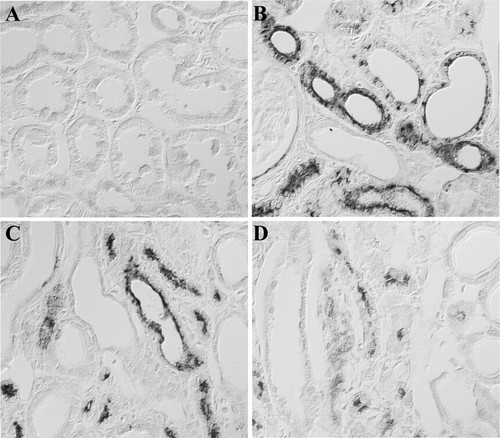
Fig. 6.Representative photomicrographs of immunohistochemistry for OPN. A: normal rat kidney. B: CsA treatment for 4 wk. C: CsA+P5 for 4 wk. D: CsA+P20 for 4 wk. Note that pravastatin significantly decreased OPN protein expression and its immunoreactivity. Immunohistochemical staining; original magnification: ×400.
Download figureDownload PowerPoint
Effect of pravastatin on TGF-β1 mRNA and protein expression in chronic CsA-induced nephropathy. CsA treatment induced a gradual increase in TGF-β1 mRNA expression at 1 (447 ± 66 vs. 105 ± 10, P < 0.01) and 4 wk (669 ± 63 vs. 103 ± 9, P < 0.01) compared with the VH group (Fig. 7), whereas the pravastatin dose dependently suppressed TGF-β1 mRNA expression at 1 (CsA+P5: 199 ± 14, P < 0.05 vs. CsA; CsA+P20: 157 ± 34, P < 0.05 vs. CsA+P5, respectively) and 4 wk (CsA+P5: 408 ± 51, P < 0.05 vs. CsA; CsA+P20: 254 ± 35, P < 0.05 vs. CsA+P5, respectively). Immunohistochemistry consistently revealed that most cortical tubules were negative for TGF-β1. In contrast, a significant increase in TGF-β1 expression was found in the CsA group, where severe fibrosis was also observed (Fig. 8). Concomitant treatment with pravastatin significantly suppressed TGF-β1 expression and immunoreactivity.
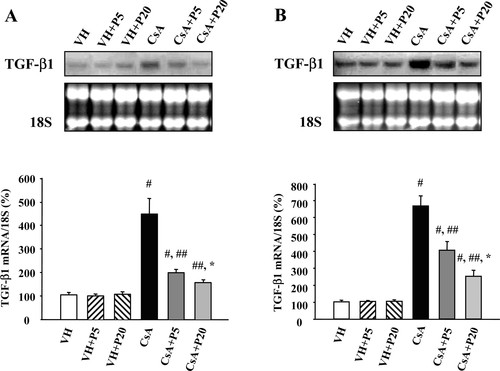
Fig. 7.Northern blotting and quantitative analysis of transforming growth factor (TGF)-β1 mRNA expression. TGF-β1 mRNA expression was significantly increased in rat kidneys with CsA treatment at 1 or 4 wk, whereas pravastatin markedly decreased its expression in a dosedependent manner. Relative TGF-β1 mRNA values are represented with the VH group designated as 100% reference and are normalized to 18S.#P < 0.01 vs. VH.##P < 0.01 vs. CsA. *P < 0.05 vs. CsA+P5.
Download figureDownload PowerPoint
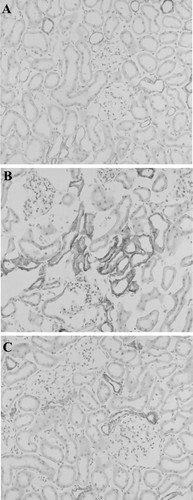
Fig. 8.Representative photomicrographs of immunohistochemistry for TGF-β1. Immunostaining was performed on cryostat sections. A: normal rat kidney. B: CsA-treated rat kidney. C: CsA+P20. Immunohistochemical staining; original magnification: ×200.
Download figureDownload PowerPoint
Effect of pravastatin on eNOS protein expression and intrarenal renin expression in chronic CsA-induced nephropathy.Figure 9 shows immunoblotting of eNOS protein. Four weeks of CsA treatment induced a dramatic decrease in eNOS protein expression (19 ± 5 vs. 104 ± 4, P < 0.01 vs. VH), whereas its expression was upregulated in accordance with the dosage of pravastatin treatment compared with the CsA group (CsA+P5: 41 ± 3; CsA+P20: 82 ± 8, P < 0.01, respectively).
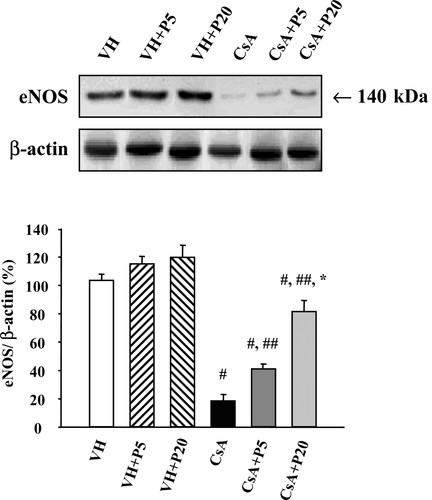
Fig. 9.Immunoblotting of endothelial nitric oxide synthase (eNOS) protein in each group. Note that CsA treatment dramatically decreased eNOS protein expression but that expression was increased in accordance with the dosage of pravastatin. The expression of eNOS protein was referenced with β-actin, and the relative optical densities (%) are presented with the VH group designated as 100%.#P < 0.01 vs. VH.##P < 0.01 vs. CsA. *P < 0.01 vs. CsA+P5.
Download figureDownload PowerPoint
We used a well-documented immunohistochemical technique for renin detection and for semiquantitative analysis of renin-positive glomeruli to represent the status of the RAS (30). Intrarenal expression of renin was minimal in the VH group, but its immunoreactivity and the number of reninpositive glomeruli significantly increased in the CsA group compared with the VH group (Fig. 10, 32 ± 3 vs. 9 ± 1, P < 0.01). Neither of the two dosage of pravastatin affected intrarenal renin immunoreactivity or the number of renin-positive glomeruli (CsA+P5: 31 ± 3; CsA+P 20: 30 ± 5, respectively).
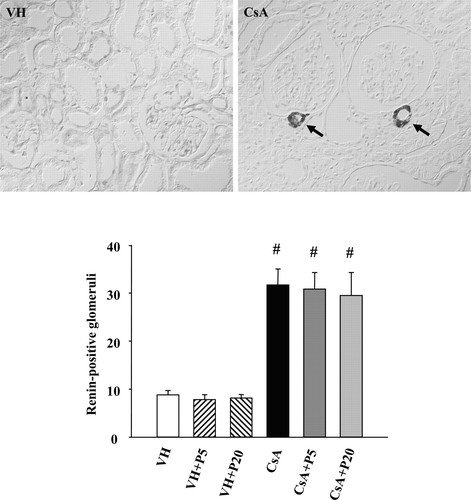
Fig. 10.Representative photomicrographs of immunohistochemistry for intrarenal renin and semiquantitative analysis of renin-positive glomeruli (arrows). CsA treatment for 4 wk significantly increased intrarenal immunoreactivity of renin and renin-positive glomeruli, but pravastatin did not influence them. Immunohistochemical staining; original magnification: ×400.#P < 0.01 vs. VH.
Download figureDownload PowerPoint
DISCUSSION
The present study clearly demonstrates that, in a rat model of chronic CsA-induced nephropathy, pravastatin attenuates tubulointerstitial inflammation and TIF probably by downregulating the expression of OPN, intrarenal CRP, and TGF-β1 and by upregulating eNOS protein expression. Interestingly, there were no significant differences in systemic lipid or CRP levels.
Pravastatin inhibits inflammatory mediators (e.g., monocyte chemoattractant protein-1 and TNF-α) and macrophage infiltration (17, 33, 34, 50) and suppresses mesangial cell proliferation, TGF-β1 expression, and extracellular matrix (fibronectin and type IV collagen) production in cultured mesangial cells (6, 38, 57). Thus pravastatin may have both anti-inflammatory and antifibrotic potential in the kidney. In the present study, we observed that pravastatin significantly decreased OPN and TGF-β1 expression and the number of ED-1-positive cells at 1 and 4 wk in accordance with the dosage administered, which was paralleled by a significant attenuation of TIF at 4 wk. However, there were no significant differences in lipid parameters in any treatment groups. Our results suggest that pravastatin suppresses the progression of tubulointerstitial inflammation and TIF through a mechanism involving decreased OPN and TGF-β1 expression in chronic CsA-induced nephropathy.
CRP is an inflammatory biomarker and a strong predictor of cardiovascular diseases and renal function abnormalities in humans (2, 51). In general, CRP is the main acute reactant, and its production is presumably restricted to the liver, but a recent study has suggested that the kidney may be a second site of CRP formation (18). In rats, CRP is not a typical acute phase protein (43), and a role for CRP is not well characterized. However, a recent publication demonstrated that rat CRP, similarly to human CRP, can activate autologous complement (41). This finding suggests that biological functions of CRP are conserved among species. In this study, we measured systemic hs-CRP level and intrarenal CRP expression to evaluate antiinflammatory effects of pravastatin on chronic CsA nephropathy. The results of this study revealed that pravastatin treatment decreased CsA-induced overexpression of intrarenal CRP expression. On the other hand, neither CsA nor pravastatin influenced serum hs-CRP concentrations in the treatment groups. On the basis of our study and previous reports, we propose that the attenuation of tubulointerstitial inflammation by pravastatin treatment in CsA-treated rat kidneys may be related, in part, to the decrease in intrarenal CRP expression.
The mechanism by which pravastatin attenuates interstitial inflammation and fibrosis in this model may be multifactorial, but two possibilities should be considered. First, chronic CsA-induced nephropathy is associated with afferent arteriolopathy (10), which ultimately leads to hypoxia-induced renal tubulointerstitial inflammation and TIF. Statins modulate vascular remodeling by inhibiting smooth muscle cell proliferation, migration, and extracellular matrix synthesis (14, 27, 44). Second, endothelial NO dysregulation has been linked with CsA-related vasoconstriction, inflammatory reaction, and fibrosis (16, 56). Recently, in vivo and in vitro studies have confirmed that statins improve endothelium function through enhancing eNOS expression and its activity (20, 28, 37). Here, we found that pravastatin significantly augmented eNOS protein expression and decreased afferent arteriolopathy. Therefore, the anti-inflammatory and antifibrotic effects of pravastatin in this study may be associated with its effects on arteriolopathy and endothelial NO.
In addition, the RAS plays an important role in the pathogenesis of chronic CsA nephropathy (55). This is supported by the observation that blockade of the RAS with either angiotensinconverting enzyme inhibitors or angiotensin type I-receptor antagonists attenuates fibrosis in chronic CsA nephropathy (3). In the present study, we evaluated the status of the intrarenal RAS using immunohistochemistry, assuming that the effect of pravastatin on chronic CsA nephropathy is mediated by inhibition of the RAS. However, we observed no significant differences in intrarenal renin immunoreactivity between the CsA and CsA+P groups. Thus it is likely that the renoprotective effect of pravastatin in this model is unrelated to the RAS, which is consistent with data from another study that indicate that pravastatin cannot influence cardiac ACE activity (37).
The types and dosage of statins are major limiting factors in the use of these drugs in clinical transplantation, because of adverse effects (myositis and rhabdomyolysis) or drug-drug interactions. Unlike lipophilic HMG-CoA reductase inhibitors, pravastatin is hydrophilic, and its metabolism is independent of that of cytochrome P-450 3A4 in the liver (53). As a result, pravastatin may have fewer toxic effects than other statins. It has been reported to be efficacious and tolerated well by transplant recipients undergoing CsA therapy (58). In the present study, we chose to compare two doses of pravastatin (5 or 20 mg/kg). Interestingly, the lower dose only improved renal histopathology, whereas the higher dose improved both histopathology and renal function. This observation suggests that, although a low dose of pravastatin (5 mg/kg) failed to overcome the hemodynamic changes caused by CsA, it was still effective in preventing the progression of chronic CsA-induced nephropathy.
The functions of pravastatin also extend to immunomodulation, as demonstrated by the inhibition of the expression of class II major histocompatibility antigens and of natural killer cell activity (52). Indeed, experimental and clinical studies in cardiac and renal transplant recipients show that the administration of pravastatin successfully decreases acute or chronic rejection episodes and improves graft survival (19, 24, 26). Furthermore, combined treatment with pravastatin and CsA produced additional immunosuppression in patients with kidney transplants (24), which was related to the synergistic inhibition of cytotoxic T lymphocyte activity (23). From this study and other reports, we suggest that adding pravastatin to CsA-based immunosuppressants may achieve enhanced immunosuppression in addition to lessening CsA-associated nephrotoxicity. Future clinical study is required to investigate this issue.
In summary, this study demonstrates that pravastatin elicits anti-inflammatory and antifibrotic effects in a rat model of chronic CsA-induced nephropathy. Suppression of OPN, TGF-β1, and intrarenal CRP expression along with higher eNOS expression may be one of the mechanisms underlying the renoprotective properties of pravastatin. Our findings provide a potential rationale for the clinical use of pravastatin in reducing chronic CsA-induced nephropathy.